Familiar themes for a novel virus
 March 26, 2020
March 26, 2020 Reflections on COVID-19 and the Corona Virus Pandemic
As panic over the new virus spread, a group of protestors marched through downtown Manhattan carrying a banner that read, “We Need Research Not Hysteria.” They were not referring to coronavirus disease (COVID-19). It was June 1983 and they were protesting the cloud of misinformation that was hampering research into a relatively new disease called “acquired immune deficiency syndrome” (AIDS).
On March 11, 2020, COVID-19 joined AIDS as the world’s second active pandemic. The two pathogens responsible for these diseases, human immunodeficiency virus (HIV) and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), are very different organisms with different pathologies. However, at the outset, the pandemics they triggered are both characterized by the same critical shortages. I’m not talking about face masks, hand sanitizer, or even toilet paper. The biggest shortage the public faces today is the shortage of reliable information about the disease.
If the HIV/AIDS pandemic has taught us nothing else, it’s that the wrong information can trigger hysteria, accelerate transmission, stall funding, delay a proper public health response, and ultimately result in otherwise avoidable loss of life. Given that, anyone in a position of leadership during a public health crisis would be well advised to take these matters to heart.
This illustration, created by the US Centers for Disease Control and Prevention (CDC), reveals ultrastructural morphology exhibited by coronaviruses. A novel coronavirus, named Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2), was identified as the cause of an outbreak of respiratory illness first detected in Wuhan, China in 2019. The illness caused by this virus has been named coronavirus disease 2019 (COVID-19).
Misinformation
No individual, organization, or government can control what information is shared. Misinformation is a result of the general confusion that surrounds any emerging infectious disease. New research and facts are published at such breakneck speed in the early days of a pandemic that it can be difficult for anyone to keep up. Just today, I rewatched an interview with a highly regarded infectious disease expert from March 5, 2020. He made perfect sense two weeks ago but about 20% of what he said has since been proven wrong.
Misinformation seems to be an unavoidable byproduct of people trying to come to grips with the nature of the pathogen they are fighting. At the outset of the HIV/AIDS pandemic, the resulting illness was given several misleading names by well-intentioned individuals based on its symptoms and similarities among its first victims. It was called “Gay Men’s Pneumonia,” “Gay Cancer,” and “Gay-Related Immune Deficiency.” Researchers would soon learn that the virus was capable of infecting any man, woman, or child. On September 24, 1983, the more accurate term “acquired immune deficiency syndrome” (AIDS) was first used by the US Centers for Disease Control and Prevention (CDC), but almost 37 years later, many of the original myths surrounding the disease persist and continue to shape public opinion.
In 1981 there was no public internet or social media. By today’s standards, news traveled slowly from one news outlet to another, sometimes crossing borders over the course of weeks. Today, information itself “goes viral” spreading around the world in a matter of hours. Well-intentioned internet users, eager to share with each other, often spread information from sources that vary wildly in validity. This isn’t malicious, its human nature. But it is why the public needs trusted, unbiased sources of information in times of crisis and why our leaders need to make a concerted effort to provide it.
Disinformation
Then, of course, there are the bad actors who seek to exploit the situation surrounding pandemics by purposely spreading false information. This is not merely a Facebook phenomenon and is not limited to politicians seeking reelection. We saw it in 1985 when the former East German secret service, the Stasi, pushed a false story that HIV was created in a US government bio-weapons lab to target certain marginalized populations and was accidentally released. They were looking to use the HIV/AIDS pandemic as an opportunity to discredit the US. The story began to spread around Europe and eventually made it to mainstream media in the US. By 1987 the story was published over 200 times in over 70 countries. I could not help but make this connection when I heard the unfounded allegations that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was likewise created and accidentally released from a Chinese bio-weapons lab in Wuhan.
Recently, students on Spring Break in the US were criticized for defiantly ignoring advice to practice social distancing as they partied in Florida. With an estimated 20% of the world’s population currently on lockdown, it’s understandable that many people were enraged with them. They were cited as an example of everything that’s wrong with young people today. But using the folly of youth as an excuse misses the real culprit. For every ER physician and global pandemic expert extolling the severity of the COVID-19 risk and the need for social distancing, there were ample pundits and politicians downplaying the threat and encouraging business as usual during the outbreak. It’s hard for people of any age to discern the real risks of a pandemic when the media is awash in contradiction. And had a student, or anyone else choosing to ignore health officials, felt the need to have their actions validated, then they could have simply cherry-picked news sources that conformed to their views and opinions. Up to now, the real-life consequences of this type of selective societal listening have mostly been political. During a pandemic it can be a matter of life and death.
Putting a positive spin on a dangerous pandemic can only make matters worse. John Barry, who wrote The Great Influenza: The Story of the Deadliest Pandemic in History, recently published an article in The New York Times. While he acknowledges that COVID-19 does not seem to be as deadly as the 1918 flu pandemic, he states that there is still much we can learn from our past. The most important lesson, he says, is to tell the truth no matter how unsettling or difficult. He says that lying about the severity of the crisis in 1918 had dire consequences. “Trust in authority disintegrated, and at its core, society is based on trust. Not knowing whom or what to believe, people also lost trust in one another. They became alienated, isolated. Intimacy was destroyed.”
Clinical Information
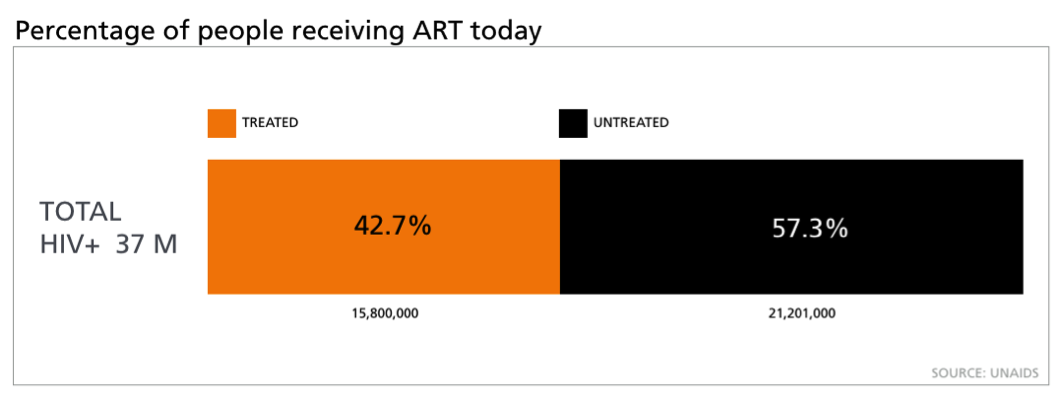
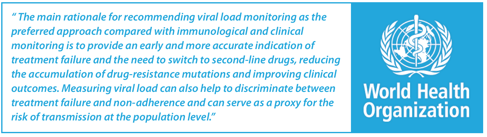
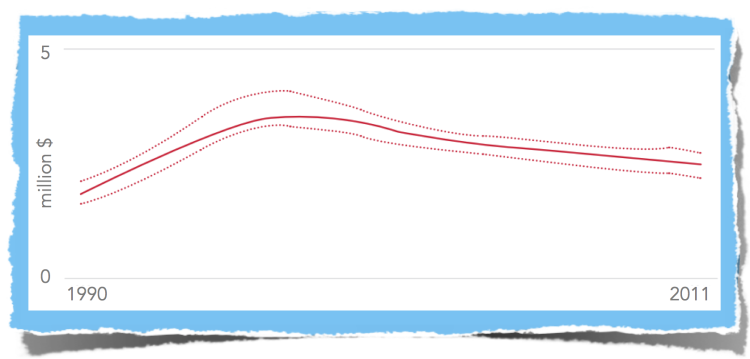
The need for reliable information does not stop even after the public comes to grips with a pandemic. It moves to care and treatment. To paraphrase business thinker Peter Drucker, you can’t manage what you can’t measure. Managing infection, whether for a population or an individual patient, relies on accurate quantification on a clinical level. This is as true for HIV/AIDS as it is for COVID-19. Universal access to tests that can reliably quantify HIV in the clinic has been an issue that has dogged treatment efforts in resource-limited settings for decades. Even when treatment is available, the inability to quantify viral load in a patient undermines outcomes in HIV-positive patients. We are just beginning this journey with SARS-CoV-2 and hopefully will benefit from lessons learned with HIV
 ZIVA™ delivers a fully-automated, immunodiagnostic platform purpose-built to meet the requirements of decentralized labs like those in district hospitals.
ZIVA™ delivers a fully-automated, immunodiagnostic platform purpose-built to meet the requirements of decentralized labs like those in district hospitals.
As with HIV/AIDS, we can anticipate that there will be an ongoing need for global, decentralized testing not only to diagnose COVID-19 but also to track disease progression for patients and populations. Today companies that provide diagnostic test kits, ventilators, and face masks are working hard to adapt to the COVID-19 pandemic. Likewise, diagnostic companies will need to do the same to ensure we have accurate information to track and manage this emerging pathogen moving forward. For example, at Cavidi we have found a way to modify our ZIVA immunodiagnostic platform to address the COVID-19 pandemic. ZIVA was designed to monitor HIV viral load with the ability to expand and accommodate other tests. The ZIVA platform could easily be adapted to provide an accurate determination of immunity to SARS-CoV-2
I’m pleased to announce that the ZIVA platform will be able to contribute to the fight against the COVID-19 pandemic. It will offer clinicians and public health authorities a deployable and highly sensitive assay to quantify IgG and IgM antibody titers. This work is straightforward and could be completed within months with adequate funding, which would have the following applications.
Peri-pandemic applications include:
- Screening first responders and providers (healthcare, police, military, etc.) for immunity so they can then be deployed without fear of infection/reinfection.
- Reducing/lifting individual movement restrictions since confirmed immune individuals would not need to observe quarantine/travel restrictions.
- Immune people could serve as a barrier to the infection to their family/friends by running the critical household errands.
- Allowing people to safely return to work if immunity is confirmed.
- Allowing for vaccine triage: the first round of vaccines will need to be rationed and knowledge of immune status due to previous infection will be crucial.
Post-pandemic applications include:
- The short-lived nature of immunity against Coronaviruses, in general, may require routine immunological testing on a scale not seen before to ensure the pandemic does not repeat itself.
- It could be used as a screening tool to select those in need of a booster vaccine.
In times of uncertainty and crisis, clear information saves lives. This is as true on a national level as it is in the clinic. As with the HIV/AIDS pandemic in 1984, medical diagnostic companies like Cavidi once again find themselves in a position to help provide that vital information to stem the tide of a global pandemic. I can give you my assurance that we do not take this responsibility lightly. Cavidi will continue to work through this current crisis to give healthcare providers the information they need to better manage this pandemic and care for their patients.