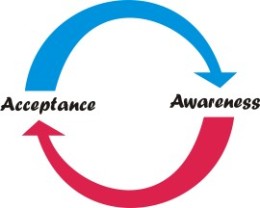
Each year World Aids Day helps raise awareness around the world. It’s also a time for everyone involved in the fight against HIV to step back and assess our progress. Looking at the HIV community as a whole and Cavidi in particular, I can say it’s been a good year overall. We have seen great progress in the treatment of HIV worldwide. At the same time, these developments have further clarified the challenges that remain to providing universal access to proper HIV treatment and prevention.
 World Aids Day Graphic from http://worldaidsdaynw.org/
World Aids Day Graphic from http://worldaidsdaynw.org/
World Aids Day 2013 marks the halfway point of UNAIDS’ Getting to Zero initiative. This ambitious initiative has three core objectives to achieve by 2015:
- Zero new HIV infections
- Zero AIDS-related deaths
- Zero HIV-related discrimination
So where does the world stand at the halfway mark? Many of the statistics coming from the WHO are cause for optimism taken at face value. But with an estimated 2 million people contracting HIV each year and over 1.5 million deaths attributed to AIDS, it’s clear that we are still a long way from zero.
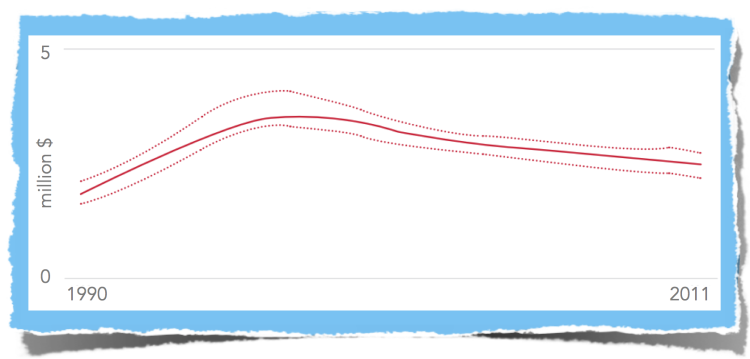
Given the complexity of these issues and the limitations of the available data, it’s often quite difficult to get a fix on where we are on our journey to zero. Roger Tatoud explains just how difficult this task can be in an excellent post he wrote a few weeks ago on the 0 Incidence blog. In his post, Roger boils down a sea of data into three clear graphs that together start to give us insight into where we stand today. I was particularly interested in his analysis of how we are doing in terms of providing access to HIV treatment. The year-on-year increase in the number of people able to access HIV treatment has been rising steadily since 2006. That’s all good. However, the rate of change year-on-year over the same period has been in steady decline, meaning that although more people are accessing HIV treatment each year, the rate at which people are accessing HIV treatment is slowing down. That’s not good. Roger concludes, “This suggests that current approaches to deliver treatment are reaching a limit (or that something is limiting further expansion) and that for treatment to reach more people more effort will be needed or that we will need to do things differently.”
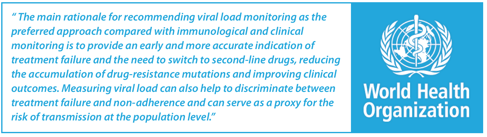
Part of that difference may well be an increased role for viral load monitoring in the treatment of HIV. 2013 saw viral load monitoring receiving increased attention among the world’s most influential healthcare bodies such as WHO, UNAIDS, UNITAID and MSF. A decade after acknowledging the importance of HIV viral load monitoring, the World Health Organization 2013 revised guidelines, calling for developing countries to roll out routine virological monitoring, with viral load tests at both six and twelve months after treatment initiation, and then at least every twelve months thereafter. In this way, treatment adherence problems are corrected more quickly and patient treatment can be adjusted if the viral infection is not responding to therapy.
This decision was further supported by a report from Médecins Sans Frontières (MSF) that highlights the importance of routine HIV viral load monitoring in low-income countries. Today, most clinics in resource-limited settings try to monitor disease progression with CD4 tests alone. The MSF research provides ten specific benefits that programs in developing nations can hope to achieve by adopting the WHO recommendation for routine HIV viral load testing. Among them are confirmation of treatment failure, prevention of HIV mother-to-child transmission, and improvement in HIV treatment outcomes in low-income countries. If realized, the benefits outlined in the MSF report would certainly move us closer to UNAIDS Getting to Zero goals.
The increased interest in viral load monitoring witnessed over the past year has been accompanied by increased interest in point-of-care solutions. The idea is to get the HIV monitoring test out to where the problem is. I sense this is a reaction to address the inadequacies of centralized testing, particularly in resource-limited settings where simply transporting samples to a central lab can be a limiting factor. While the point-of-care initiatives are a welcome development to dysfunctional centralized options, there is middle ground that needs to be kept in mind.
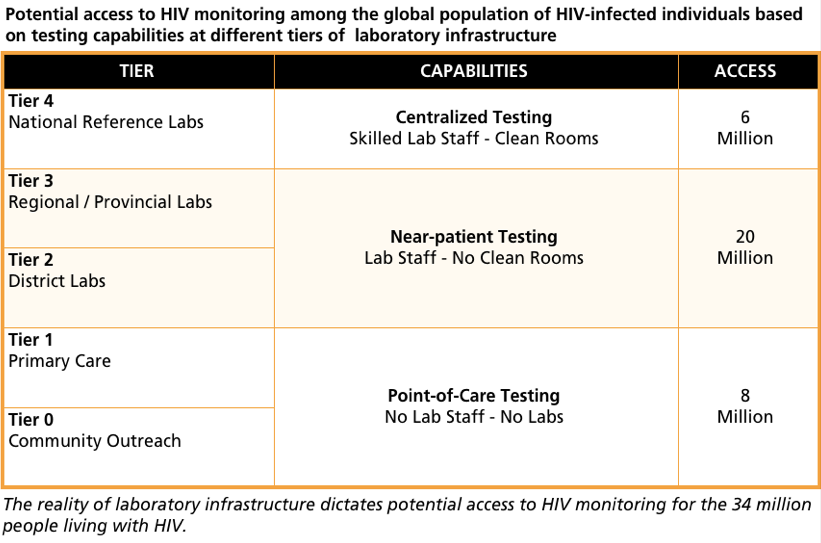
Any solutions for HIV treatment have to work with the realities of existing laboratory infrastructure. The WHO has designated five tiers of laboratory infrastructure. Each has its capabilities in terms of what types of tests can be run and the throughput that is possible. This, in turn, influences the access to testing that we can expect from any tier. For instance Tiers 0 and 1 may interact with a large population of people living with HIV, but since there is no lab infrastructure and a shortage of skilled staff exists at that level, testing is limited to one-at-a-time, point of care testing with low throughput. We have drawn on throughput projections and population geography to provide a picture of potential access to monitoring at the different levels.
If we estimate the global population of people living with HIV to be at around 34 million, we can divide them by this type of access. There we see that the centralized testing schemes used by reference labs in Tier 4 could access about 6 million people living with HIV and this is where, traditionally, much of the emphasis has been placed. Primary care facilities and community outreach programs in Tier 0 and 1 could reach about 8 million people living with HIV and this is where point-of-care solutions can have the greatest impact. But with near-patient testing, regional and district-level facilities in Tier 2 and 3 could provide access to over 20 million or 60 % of cases. Today, Cavidi’s ExaVir™ Load test is the only test capable of providing viral load monitoring coverage on a regional and district level.
These middle tiers are where Cavidi focuses its efforts both with our current product, ExaVir™ Load, and with our R&D efforts to develop new monitoring solutions that will increase throughput and access even further. I’m pleased to announce that we have made significant progress in both areas over the past year.
In 2013 we reached another milestone with our ExaVir™ Load HIV viral load monitoring kit as we began shipping to the Philippines. This marks the 25th country to adopt ExaVir™ Load for clinical use in addition to over a dozen other countries where the test is currently being evaluated for use. The test offers the same sensitivity and accuracy of Tier 4 reference tests but, unlike those tests, it can be run in Tier 2 and 3 facilities – and at a fraction of the cost.
 Cavidi’s new Automated Monitoring System will provide viral load and be adding other optional HIV test kits, such as CD4, EID, and drug resistance in one robust bench-top unit.
Cavidi’s new Automated Monitoring System will provide viral load and be adding other optional HIV test kits, such as CD4, EID, and drug resistance in one robust bench-top unit.
We are also making steady progress on the next generation of HIV viral load monitoring diagnostics. Codenamed the Automated Monitoring System, the new system is now in the prototype stage. This new product uses the same proven RT-technology found in our ExaVir™ Load test but it is fully automated, requiring less time from lab technicians and greater throughput. In addition to viral load testing, we will be adding other optional HIV test kits like CD4, EID, and drug resistance in one bench-top unit. Like ExaVir™ Load, our new system is ideally suited to the near-patient testing needs of Tier 2 and 3 regional and district level facilities. Bringing this product to market will be a game changer for increasing both access and quality of HIV treatment globally. I look forward to sharing more news on the project throughout 2014.
While 2013 saw progress in the battle against HIV, it’s clear that we still have lots of work ahead of us. That’s why we need to ensure that the public remains aware and vigilant. My colleagues and I at Cavidi will continue to work to increase awareness, access, and quality of HIV treatment worldwide. In the interest of raising awareness among your peer network, I hope you will share this post. If you would like more information about Cavidi’s work in this area, feel free to contact me directly.
 November 30, 2014
November 30, 2014  The time for viral load testing is now.”For years this has been the focus of this company and each of our employees. Today, it has become policy for developing nations around the world as recommended by the World Health Organization (WHO).
The time for viral load testing is now.”For years this has been the focus of this company and each of our employees. Today, it has become policy for developing nations around the world as recommended by the World Health Organization (WHO).